
Postmenopausal Bleeding on Hormone Therapy: Practice Pearls
The endometrial lining of a postmenopausal patient is inactive and thus free of cyclical changes that are characteristics of the reproductive years. This inactivity leads to atrophy which may result in abnormal and recurrent uterine bleeding.1 Postmenopausal bleeding warrants a full clinical work-up to rule out an underlying endometrial malignancy.1 Hormone therapy (HT) can promote a more stable endometrial lining and reduce menopausal atrophy. However, patients receiving hormone therapy, regardless of method–including subcutaneous pellets—are at an increased risk of bleeding. In fact, it is estimated that more than 40% of women will spot or bleed when initiating or altering their HT with estrogen.2
Understanding the build-up and breakdown of the endometrial lining of the uterus and the natural menstrual cycle is key. Estrogen builds the lining of the uterus during pre-ovulation (the proliferative phase), then after ovulation (during the luteal phase) progesterone becomes the dominant hormone. Progesterone is produced by the corpus luteum and helps to mature the endometrial lining—preparing it for implantation. In the absence of pregnancy, the corpus luteum decays, causing progesterone to fall which leads to shedding of the lining (menstrual bleed). It is the balance of both estrogen and progesterone that maintains stability of the endometrial lining. Thus, an excess of estrogen, or lack of progesterone may cause bleeding—and in the same light, a lack of estrogen, or an excess of progesterone may cause bleeding. Thus when providing exogenous hormones for relief of menopausal symptoms, we must do our best to maintain that balance.
Leading up to the cessation of menses is the perimenopause—where there is irregular production of both estrogen and progesterone. As such, use caution when initiating estrogen in perimenopausal patients as it may make the bleeding worse due to excess estrogen. You will see that the FSH may be high in the menopausal range, but frequently the estradiol is also high—usually above 30. The patient’s menstrual history will also likely be irregular. It is important to use the lowest amount of estrogen (6mg) and adjust or cycle progesterone to regulate the bleeding. You may even consider using just testosterone in these perimenopausal patients until all menstrual cycle/spotting has stopped for at least 6 months or more.3 Importantly, all patients started on estrogen with a uterus must receive progesterone to protect the uterus. Progesterone opposes the effect of exogenous and endogenous estrogen on the endometrium, resulting in a lower risk of endometrial cancer.[iv] Thus, patient history and progesterone are critical in a smooth start or transition with HT.
Progesterone is best absorbed with food—ideally at dinner because of its somnolent effect. The initial dose should be 225 mg compounded micronized progesterone. Be aware that if you write a generic prescription for 200 mg progesterone for your local pharmacy, it can vary by 30% and that variation in individual pill potency may lead to a withdrawal bleed, due to the imbalance of hormones.
If bleeding occurs in a postmenopausal patient, increase the progesterone to 2 pills (ideally 225 mg compounded for purity) for 10 days, then stop for 3-5 days to mimic the luteal phase of the menstrual cycle. The bleeding will frequently, but not always, slow, then during the 3-5 day break, a full shedding of the endometrial lining will occur—essentially resetting the endometrium to baseline (referred as a hormonal D&C). Then restart the one pill (225 mg compounded or 200 mg) regimen again.
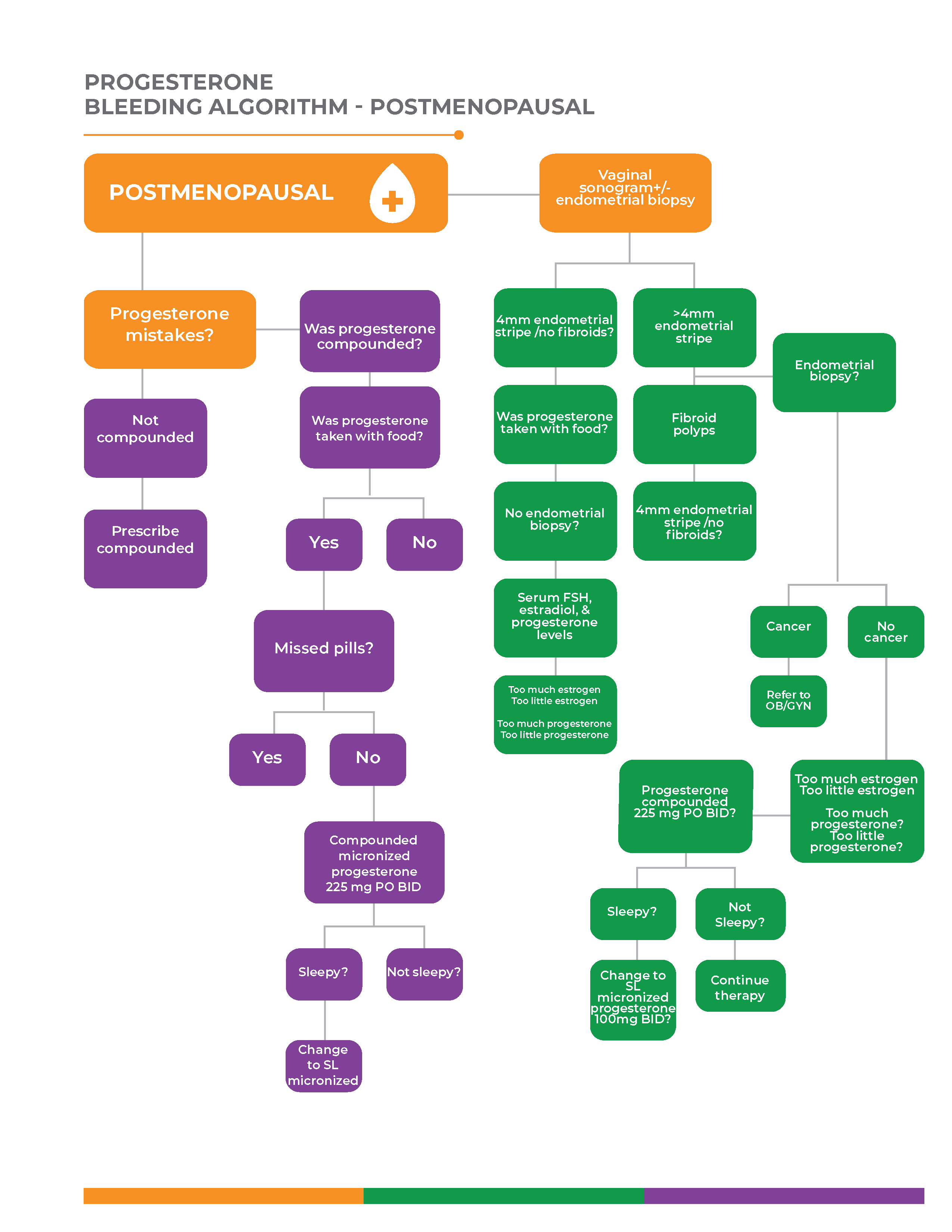
Figure 1 is the Biote-provided Decision Trees when evaluating postmenopausal bleeding.
The left side of the tree focuses on the potential mistakes associated with progesterone that may lead to abnormal bleeding. While the right side depicts the proper work-up of abnormal bleeding in a postmenopausal patient on hormone therapy.
The right side follows the use of ultrasound to rule out anatomic causes, such as polyps or fibroids and most importantly a malignancy. The use of a 4mm cut-off for the endometrial stripe by ultrasound rules out cancer >95% of the time.5,6 With a stripe greater than this or when bleeding persists, an endometrial biopsy or GYN referral and work up is required.
If the biopsy is negative, the cause of the bleeding is due to an imbalance of estrogen and progesterone.1 In the case of too much estrogen, the endometrial biopsy will reveal benign, proliferative changes. Treatment includes increasing the progesterone by the 225 mg x 2 (as described previously) and lower the estrogen dose with the next pellet insertion. In the case of too little estrogen, the endometrial stripe will be thin. Treatment includes stopping the progesterone for 1-2 weeks and increasing the estrogen dose at the next pellet insertion—depending on the timing and dosing of your patient. If the bleeding persists longer than 1-2 episodes, it is important to perform an endometrial biopsy or GYN referral to avoid missing a malignancy.
Figure 1
- Brenner PF. Differential diagnosis of abnormal uterine bleeding. Am J Obstet Gynecol. 1996 Sep;175(3 Pt 2):766-9.
- Lethaby A, Suckling J, Barlow D, Farquhar CM, Jepson RG, Roberts H. Hormone replacement therapy in postmenopausal women: endometrial hyperplasia and irregular bleeding. Cochrane Database Syst Rev. 2004;(3):CD000402.
- Monroe, Malcom G, et al “The FIGO classification of causes of abnormal bleeding in the reproductive years”, Fert and Stern Volume 95, issue 7 p2204-2208
- Key TJ, Pike MC. The dose-effect relationship between ‘unopposed’ oestrogens and endometrial mitotic rate: its central role in explaining and predicting endometrial cancer risk. Br J Cancer. 1988;57:205–212
- Kim MJ, Kim JJ, Kim SM. Endometrial evaluation with transvaginal ultrasonography for the screening of endometrial hyperplasia or cancer in premenopausal and perimenopausal women. Obstet Gynecol Sci. 2016 May;59(3):192-200.
- Gupta JK, Chien PF, Voit D, Clark TJ, Khan KS. Ultrasonographic endometrial thickness for diagnosing endometrial pathology in women with postmenopausal bleeding: a meta-analysis. Acta Obstet Gynecol Scand. 2002 Sep;81(9):799-816.
