
Decoding Perimenopause Part III: The Hormonal Rollercoaster and Risk for Pregnancy
Although conception is less likely as menses become erratic, pregnancies do occur during the perimenopause. Because cycles are irregular, it becomes difficult to determine fertile times of the cycle. The chance of pregnancy is 10% ages 40-44, 2-3% ages 45-49. “There’s no way that I could be pregnant!” is a refrain we hear not infrequently from patients in their 40s. In a recent survey, 49% of all pregnancies were unintended, but almost half of them occurred in people between the ages of 40-44.1,2 Spontaneous pregnancies have been achieved as late as age 54. In addition, 84% of pregnancies in women over 48 ends in first trimester loss and the risk of an ectopic pregnancy in women over 44 rises to 7%.3
Pregnancy should be your top concern when a perimenopausal patient presents with abnormal bleeding. Perform a pregnancy test as your first step in management. Abnormal bleeding is one of the most common presenting complaints encountered in a gynecologist’s office or primary-care setting. Women with menstrual-related problems are more likely to report anxiety, depression, insomnia, excessive sleepiness, and pain than women without menstrual-related problems—confusing the hormonal situation further!4
For your perimenopausal patient, the bleeding accompanies menopausal symptoms and because of this, many providers are quick to want to use estrogen. As discussed in Part I and II of this Perimenopause series, it is the imbalance between estrogen and progesterone that is the cause and ultimately it is progesterone that can help these patients. As such, a discussion regarding birth control is essential.
A combined estrogen/progestin oral contraceptive (COC) is an excellent choice to cover the irregular bleeding, progesterone deficiency/estrogen dominance, and birth control at the same time. Taking COCs can help control these symptoms and significantly reduce the risk of ovarian cancer, endometrial cancer, and colorectal cancer.5-8 However, combined oral contraceptives can adversely affect coagulation, gallbladder function, and blood pressure. Progestins, because of their structure can stimulate not only progesterone receptors, but also glucocorticoid receptors, cortisol receptors and block androgen receptors. The resultant side effects can be nausea, bloating, weight gain, headache, fatigue, and depression. The major complications of COCs seem to be deep vein thrombosis, pulmonary embolism, heart attack and stroke. Due to their metabolism in the liver, COCs increase sex hormone binding globulin (SHBG) which can decrease effective testosterone and thyroid hormone levels.
For some patients, a better choice may be progestin only contraceptives (POC). This can come in the form of tablets, progestin containing IUD’s, injections, or an implant. Progestin-only pills include Norethindrone and Drospirenone containing formulations, which differ in their ability to suppress ovulation. Norethindrone pills contain 350 µg of norethindrone compared with 1000 µg in a typical combined contraceptive pill. The lower amount of progestin in norethindrone pills results in less consistent ovulation suppression and more potential for breakthrough bleeding. The contraceptive efficacy is maintained by other progestin-mediated effects. Drospirenone-only pills contain slightly more progestin than an estrogen and progestin combined hormonal contraception, which aids in ovulation suppression.9
Recall that progesterone is the only naturally occurring progestin; most contraceptive progestins, such as levonorgestrel and norethindrone, are synthesized from testosterone. Progestins provide a contraceptive effect by suppressing gonadotropin-releasing hormone from the hypothalamus, which lowers luteinizing hormone from the pituitary, and in turn prevents ovulation. They also thicken cervical mucus and prevent sperm from accessing the upper female genital tract.
Estrogens enhance contraceptive effectiveness by suppressing gonadotropins and follicle-stimulating hormone, preventing the development of a dominant follicle. However, the most important contribution of estrogens to progestin-based contraceptives is the reduction of irregular bleeding. The estrogen component in most combined hormonal contraceptives is ethinyl estradiol.
Combined hormonal contraceptives prevent pregnancy through the same mechanisms as progestin-only methods. Their greatest advantage over progestin-only methods is their ability to produce a consistent, regular bleeding pattern.
What do you need to warn your patients about?
In 2016, the CDC presented guidelines, called the Medical Eligibility Criteria, based on the current published evidence, regarding which contraceptive methods can be used safely when various medical conditions are present10. In these guidelines, the only age restriction on the use of COCs mentioned is for women aged 35 years or older who smoke 15 or more cigarettes per day. Thus, age itself is not a contraindication for COCs, and the guideline mentions that COCs can be used until menopause. Although COCs increase the risk of, VTE, stroke and MI, the additional events are rare, even for patients in their 40s. Therefore, perimenopausal women can safely use COCs, if they do not smoke, do not have migraine with aura (which increases the risk of stroke) and have normal blood pressure with no cardiovascular disease. Patients at increased risk of thrombosis can be provided a progestin-only, non-estrogen-containing method because this method of contraception does not increase risk of venous thromboembolism.11. Progestin-only long-acting methods, such as the levonorgestrel (LNG) IUD and the subdermal implant, have typical effectiveness rates of less than 1 pregnancy per 100 women per year-similar to permanent methods, such as tubal ligation or vasectomy making them an ideal choice for a perimenopausal patient. The etonogestrel subdermal implant is effective for up to 5 years and is easily placed and removed. Initiation and discontinuation require in-person visits. The bleeding profile of the implant is less predictable and up to 11% of users remove it in the first year due to irregular bleeding.
Estrogen doses in COCs are 4–7 times higher than in menopause-specific regimens. As a result, continuing to use COCs during menopause may lead to unnecessarily high health-related risks in menopausal women12. When patients are currently using hormonal contraceptives, assessing menopausal status is more challenging as amenorrhea may be caused by the pill. Many of today’s newer low dose COCs lead to a 60% no bleeding rate, when taken as directed. Although hormonal testing is not definitive, Expert Opinion suggests that combining FSH levels with age can assist with assessing menopausal status in women using hormonal contraceptives between the ages of 50 and 55 years old.13 See Figure 1.
Figure 1
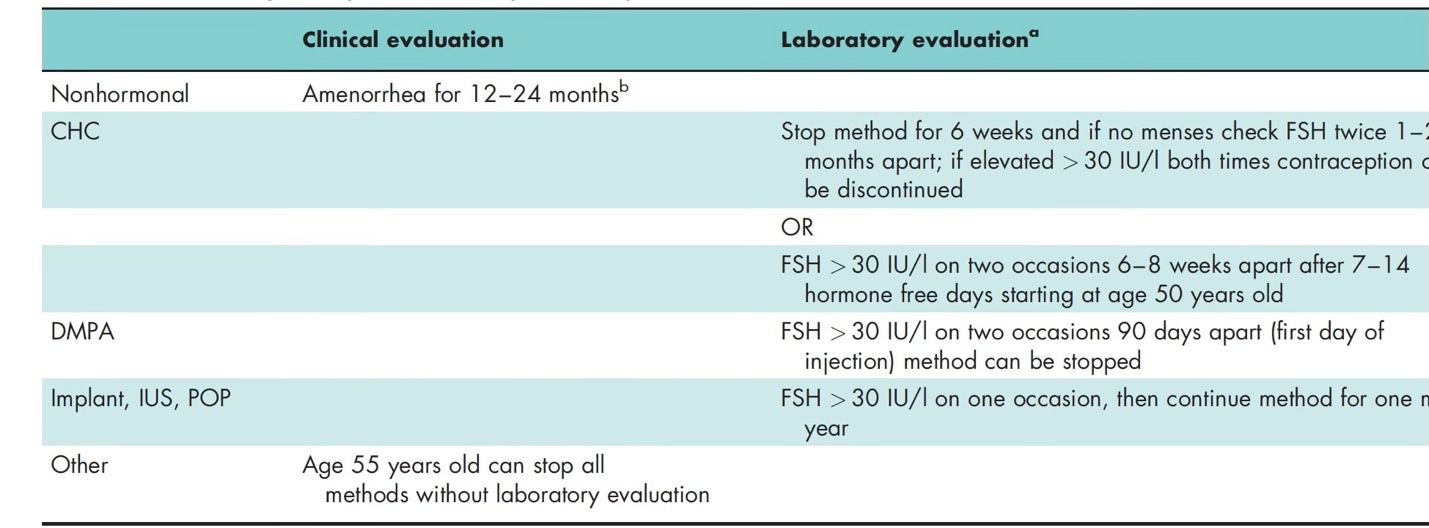
The key in stopping hormonal birth control for assessment is to counsel to use an alternate form of birth control to avoid an undesired pregnancy. Barrier methods such as condoms or a diaphragm with or without a spermicide are frequently the choice. One may also consider a non-hormonal IUD.
Regarding changing to HRT, for women using progestin only pills (except for Drospirenone only POP’s), Nexplanon implant or LNG-IUS, clinicians can check FSH levels once; if it is more than 30 IU/l, the method should be continued for one more year and then can be safely stopped and the patient considered menopausal. If the level is less than 30 IU/l, the method should be continued for another year before rechecking FSH again.14,15 According to Expert Opinion, these methods can also be stopped at the age of 55 years without any hormonal evaluation. See Figures 2 & 3.
Figure 2
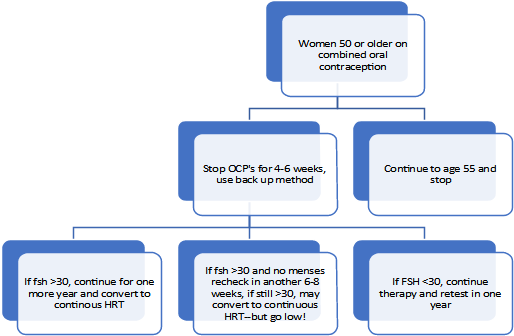
Figure 3

For women under age 50, to be safe, continue or use a copper IUD, barrier method, progesterone only oral contraceptives and look for the amenorrhea for 12 months16.
In summary, be mindful of the risk of pregnancy in your perimenopausal patient. COC’s can be helpful with preventing some cancers, regulating bleeding, and decreasing anxiety about an unintended pregnancy. Unfortunately, the negatives of interference with testosterone and libido can be difficult. Consider a hormonal IUD, which can decrease or regulate bleeding without the negative side effects of COC’s and you can more readily check menopausal status. Your testosterone therapy may be more effective without the larger hormonal interference.
References
- Andersen, A et all “Maternal age and fetal loss: Population based register linkage study. BMJ 2000; 320: 1708-1712
- Grandi G, Di Vinci P, Sgandurra A, Feliciello L, Monari F, Facchinetti F. Contraception During Perimenopause: Practical Guidance. Int J Womens Health. 2022 Jul 15; 14:913-929. doi: 10.2147/IJWH.S288070. PMID: 35866143; PMCID: PMC9296102.
- Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011 Nov;84(5):478-85. doi: 10.1016/j.contraception.2011.07.013. Epub 2011 Aug 24. PMID: 22018121; PMCID: PMC3338192.
- Strine TW, Chapman DP, Ahluwalia IB. Menstrual-related problems and psychological distress among women in the United States. J Womens Health (Larchmt) 2005; 14:316–323.
- 5. Collaborative Group on Epidemiological Studies on Endometrial Cancer. Endometrial cancer and oral contraceptives: an individual participant meta-analysis of 27,276 women with endometrial cancer from 36 epidemiological studies. Lancet Oncol. 2015;16:1061–1070.
- Collaborative Group on Epidemiological Studies of Ovarian Cancer. Beral V, Doll R, Hermon C, Peto R, Reeves G. Ovarian cancer and oral contraceptives: collaborative reanalysis of data from 45 epidemiological studies including 23,257 women with ovarian cancer and 87,303 controls. Lancet. 2008;371:303–314.
- Lurie G, Wilkens LR, Thompson PJ, McDuffie KE, Carney ME, Terada KY, et al. Combined oral contraceptive use and epithelial ovarian cancer risk: time-related effects. Epidemiology. 2008;19:237–243.
- Bosetti C, Bravi F, Negri E, La Vecchia C. Oral contraceptives and colorectal cancer risk: a systematic review and meta-analysis. Hum Reprod Update. 2009;15:489–498.
- Teal S, Edelman A. Contraception Selection, Effectiveness, and Adverse Effects: A Review. JAMA. 2021 Dec 28;326(24):2507-2518. doi: 10.1001/jama.2021.21392. PMID: 34962522.
- Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep. 2016; 65:1–103
- Tepper NK, Whiteman MK, Marchbanks PA, James AH, Curtis KM. Progestin-only contraception, and thromboembolism: a systematic review. Contraception. 2016;94(6):678-700
- Cho MK. Use of Combined Oral Contraceptives in Perimenopausal Women. Chonnam Med J. 2018 Sep;54(3):153-158.
- Baldwin MK, Jensen JT. Contraception during the perimenopause. Maturitas. 2013;76(3):235–242. doi: 10.1016/j.maturitas.2013
- Inal MM, Yildirim Y, Ertopcu K, Avci ME, Ozelmas I, Tinar S. Effect of the subdermal contraceptive etonogestrel implant (Implanon) on biochemical and hormonal parameters (three years follow-up). Eur J Contracept Reprod Health Care off J Eur Soc Contracept. 2008;13(3):238–242
- Halmesmäki K, Hurskainen R, Tiitinen A, et al. A randomized controlled trial of hysterectomy or levonorgestrel-releasing intrauterine system in the treatment of menorrhagia-effect on FSH levels and menopausal symptoms. Hum Reprod Oxf Engl. 2004;19(2):378–382.
- Faculty of Sexual & Reproductive Healthcare. Contraception for Women Aged Over 40 Years [Internet]. 2017. Available at: e https://www.fsrh.org/standards-and-guidance/documents/fsrhguidance-contraception-for-women aged-over-40-years-2017/. [September 14, 2020].
