

Decoding Perimenopause Part I*: Strategies for Diagnosis and Management
DEFINTION OF KEY TERMS
Menopause– cessation of menses for 12 months, associated with elevated FSH, low Estradiol and vasomotor symptoms in some people
Premature Ovarian insufficiency: menopause prior to age 40
Early Menopause: menopause between the ages 40-45
Perimenopause: the period of variable cycles lasting 8-10 years through 1 year after the last menstrual period
Surgical menopause: surgical removal of the ovaries with or without the uterus
“The only constant in life is change” Heraclitus, Greek Philosopher
No time can be more challenging for both women and their providers than the 10 years or so that mark the transition from regular ovulatory menstrual cycles through the year after the last period—the perimenopausal transition.
Females are born with all the primordial eggs they will ever produce. At birth, the normal female ovary contains about 1-2 million/oocytes (eggs). There is a continuous decline in the total number of eggs each month. By the time a girl enters puberty, only about 25% of her lifetime total egg pool remains, around 300,000. By the life stage of perimenopause, around age 40, the number of eggs available for stimulation and subsequent ovulation has diminished to 3% of the total egg pool with which she was born.
Perimenopause is the transition from regular ovulatory menstrual cycles through intermittent spurts of oligo-ovulation and ending with the final menstrual period. It typically lasts 8-10 years. As the onset of menarche is a process, with gradual maturation of the hypothalamic-pituitary-ovarian axis, the transition to menopause is a long process with gradual loss of follicles resulting in resistance of the ovaries to pituitary stimulation. The transition to the final menstrual period is marked by the rollercoaster of fluctuating cycles of estrogen deficiency and dominance. As estrogen levels decline, follicle stimulating hormone (FSH) rises to stimulate the ovaries into producing more estrogen. In the absence of ovulation, and therefore progesterone, there is commonly a dramatic increase in estrogen as the ovaries still respond to FSH. The irregular and unpredictable ovulation during this time leads to irregular progesterone production, which in turn leads to irregular bleeding. In addition to irregular bleeding, common symptoms of menopause may ensue…night sweats, hot flashes, sleep disturbances, irritability or mood concerns, joint pain, memory fogginess…. just to name a few. The resulting estrogen excess may also lead to bloating, breast and/or nipple tenderness, headaches and edema.
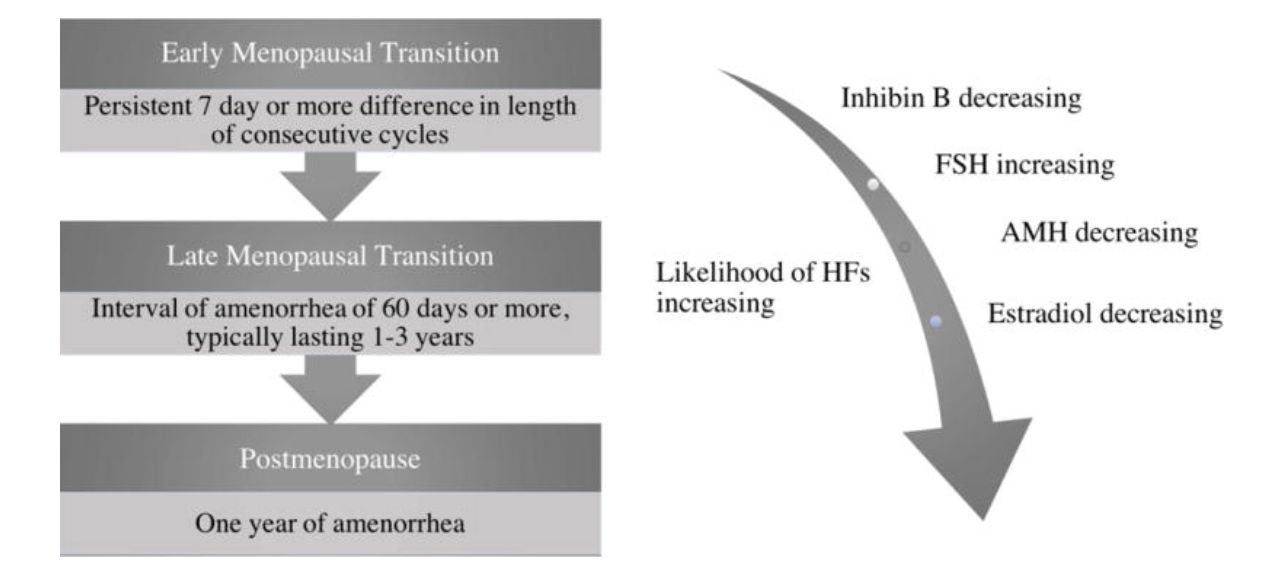
Figure 1– used from Delamater L, Santoro N. Management of the Perimenopause. Clin Obstet Gynecol. 2018 Sep;61(3):419-432.
During the perimenopausal transition, laboratory values can be difficult to interpret. Classic for menopause is a rise in FSH, frequently above 30 IU/L, with a low estradiol under 20 pg/ml—but this can fluctuate significantly in the perimenopause, and one value in time is not adequate to make a diagnosis to determine HRT and contraception needs.[1]
The STRAW (Stages of Reproductive Aging Workshop) staging of menopause is a system used to classify the various stages of a woman’s reproductive aging process.[2] It provides a framework for understanding the transition from pre-menopause to post menopause. The STRAW staging includes the following key stages:
- Reproductive Stage: This is the beginning of a woman’s reproductive life, marked by the onset of menstruation (menarche). It typically starts during adolescence.
- Early Menopausal Transition: During this stage, women may experience irregular menstrual cycles and subtle hormonal changes. Menstrual periods may become less predictable in timing and amount of flow.
- Late Menopausal Transition: In this stage, menstrual irregularity becomes more pronounced, and women often experience symptoms like hot flashes and night sweats.
- Early Post menopause: This stage is defined as the time when a woman has not had a menstrual period for 12 months. Hormonal changes are more evident, and symptoms like hot flashes can continue.
- Late Post menopause: This is the stage after several years of no menses. Symptoms like hot flashes tend to diminish, and women are at higher risk for health issues like osteoporosis and cardiovascular disease.
The STRAW staging system is a useful tool for healthcare professionals to assess and communicate a woman’s menopausal status and better understand the changes she may be experiencing during this natural life transition. It helps in tailoring appropriate healthcare and interventions based on the specific stage of menopause.
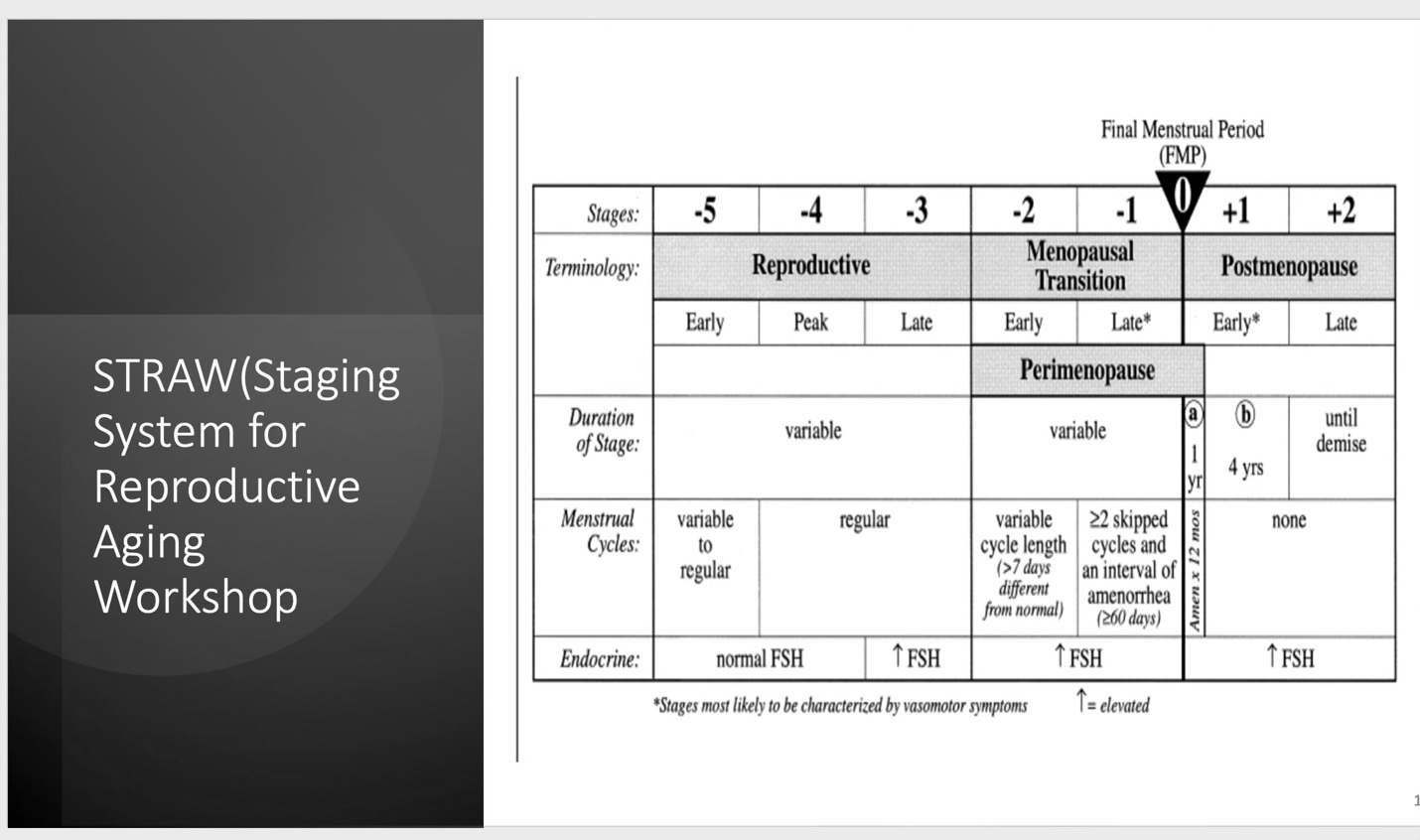
Figure 2 Summary of STRAW and staging
The SWAN (Study of Women Across the Nation) study followed a cohort of women over many years and chronicled the symptoms that accompany menopause, concomitant biological, psychological, behavioral, and social changes that come along with this transition and their ongoing health.[3] The study outlines the major categories of symptoms that affect women through the menopause transition (MT) or perimenopause. SWAN has provided valuable insights into perimenopausal and menopausal symptoms, risk factors for diseases like osteoporosis and heart disease, and the impact of lifestyle choices on women’s health. It has contributed to the development of evidence-based recommendations for women’s health care during and after menopause. You may view the Swan study fact sheets here. https://www.swanstudy.org/wps/wp-content/uploads/2023/04/SWAN-Fact-Sheets-2023.pdf
Authorities suggest that there are as few as 40 and as many as 100 different symptoms of menopause which begin prior to the final menstrual period, during the perimenopausal phase. The following is a list of symptoms noted by various sources:[1]
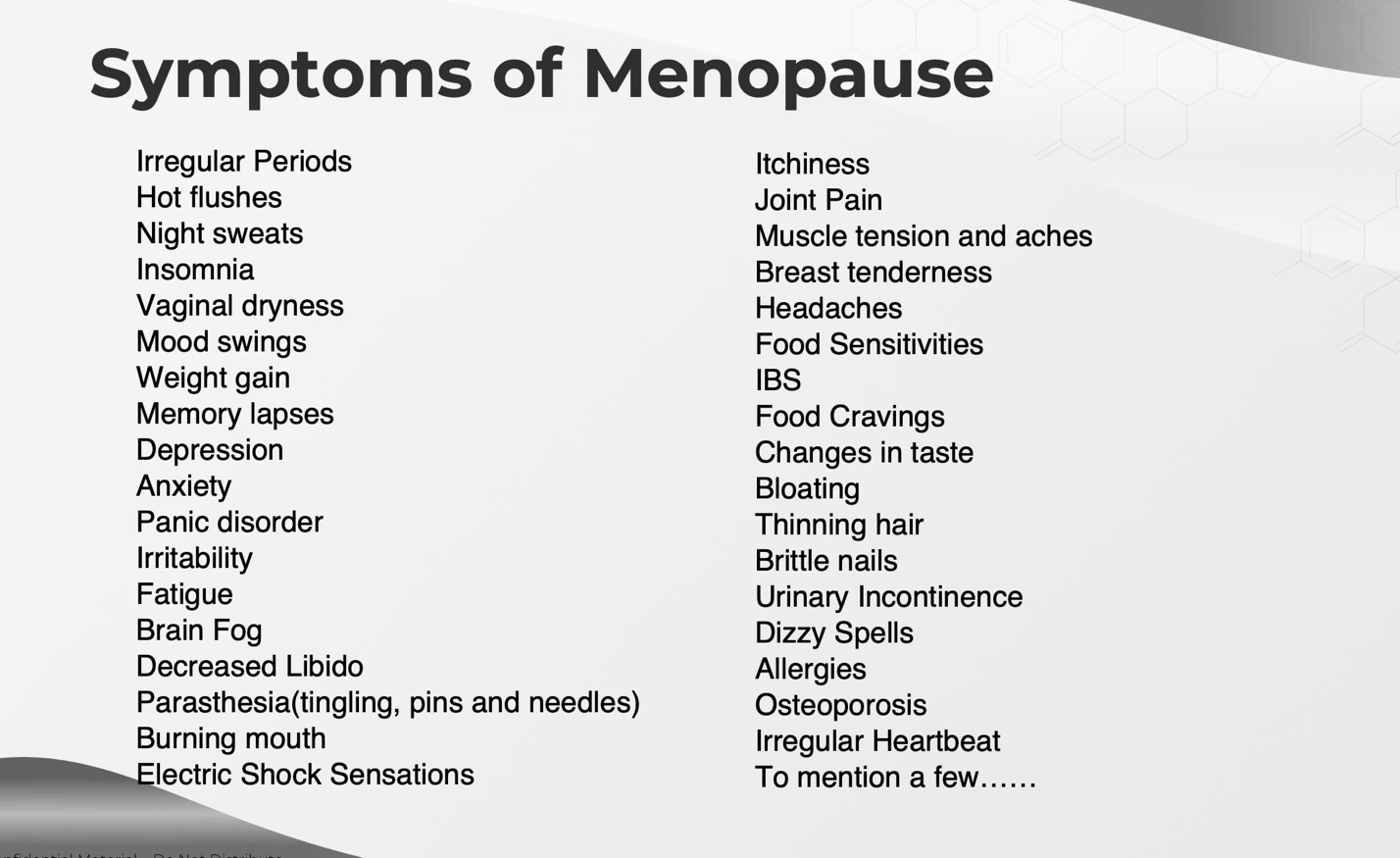
Figure 3—Symptoms of Menopause
Bleeding
Bleeding may be the most distressing issue facing the perimenopausal patient and the provider, with 77% of women having at least 3 episodes of 10+ days of bleeding during the menopausal transition [5].
Abnormal uterine bleeding presents a unique challenge to the provider in the perimenopause, as physiologic hormonal changes may mimic, or mask worrisome pathology. These presentations often warrant further evaluation to rule out serious conditions such as hyperplasia or cancer, and to guide treatment options.
General principles of perimenopausal bleeding:
- Amenorrhea is challenging to evaluate for people in their late 30s and 40s – it may reflect hypothalamic amenorrhea, polycystic ovarian syndrome (PCOS) and anovulation or early menopausal transition. For those at risk for unintended pregnancy, suppression of the hypothalamic-pituitary axis with hormonal contraception may successfully manage both the hormonal rollercoaster and the need for contraception.
- People after hysterectomy with ovarian preservation, those after endometrial ablation with resulting amenorrhea, and those with amenorrhea secondary to hormonal contraception (levonorgestrel-LNG IUD) are also difficult to diagnose. Best practice is to treat symptoms and not be concerned with a definitive diagnosis of menopause. These patients may be started on low dose (3-6mg estradiol in pellets) depending on symptoms.
- The Levonorgestrel (LNG) IUD is a practical and highly effective method for protection of the endometrium, so treating perimenopausal symptoms with low dose of systemic estradiol is reasonable as long as the IUD remains in place.
- It is very important to remember that contraception is necessary in the perimenopausal patient who is not interested in more children as intermittent and unpredictable ovulation occurs.
Bone Health
Rapid bone loss starts one year before the final menstrual period-most notably when there has been no menses for 3 or more months (in people who do not have chronic anovulation and PCOS) but some bleeding in the last year [6]. In the initial 3 years of menopause there is rapid decline in bone mineral density followed by a slower decline, at a rate of around 2% each year. [7]. In general, there are greater declines in bone density at the spine than in the hip. Over 10 years, cumulative bone density decline is around 10% [8]. In addition to bone loss, loss of bone quality and strength (the ability to resist breakage or fracture) occurs during this time[8,9]. Greater bone density loss during the menopausal transition (MT) is correlated with more fractures in postmenopausal women. [9].
Vasomotor symptoms (VMS)
VMS are sudden, intense sensations of warmth often involving the face, and upper torso, sometimes followed by chills. It was long thought these were caused by low estradiol, but they are most strongly correlated with high FSH.[10]
Up to 80% of women experience VMS during the perimenopause. Women in the SWAN study who experienced VMS in the pre or perimenopausal time frame had symptoms for a median duration of 11.8 years![11]. Results of the SWAN study have demonstrated that symptoms vary by ethnicity. Overall, median duration for VMS was 7 to 10 years. However, African American women were found to have the longest median duration of 10.1 years compared to 8.9 years for Hispanic women, 6.5 years for non-Hispanic white women, 5.4 years for Chinese women and 4.8 years for Japanese women[13,14]
Other factors that impact risk for and severity of symptoms include body-mass index (BMI), cigarette smoking, depression, anxiety, and alcohol intake[12,15]. In the SWAN study, women with a high BMI noted worse VMS during the menopausal transition, but milder symptoms after the final menstrual period (FMP)[15]
Cardiovascular disease (CVD) is the number one killer of women and the risk increases significantly in the peri and menopausal years. Frequent VMS has been shown to correlate with an increased risk of developing CVD over a 14 year period; this finding was demonstrated in women reporting later onset VMS as compared to those experiencing them in the early menopausal transition[16, 17]
Genitourinary Syndrome of Menopause (GSM)
Vaginal changes such as dryness and atrophy that may lead to dyspareunia and bothersome urinary symptoms affect up to 1/2 of women in menopause, but can start in the perimenopause. These symptoms, collectively, are termed genitourinary syndrome of menopause(GSM). Decreasing estrogen results in decreased vaginal collagen and elastin content, thinned epithelium, and increased vaginal pH [18].
This may have a significant negative effect on sexual function in those who are sexually active. In fact, a decrease in sexual function is commonly reported up to 20 months prior to the final menstrual period, and 40% of women with GSM report some type of sexual dysfunction[19, 20]
Physical Function Decline
Women with surgical or naturally occurring menopause have a 4-fold greater odds of physical function limitations. This is adjusted for age ethnicity, education and health factors. An accelerated decline in strength starts in the perimenopause. This risk of decline is higher if the patient has diabetes, hypertension, arthritis, or depression.[21]
Sleep and Mood Changes
Difficulty with sleep can be one of the most common and troubling symptoms of the perimenopause. The symptoms may include difficulty falling asleep, early awakening, and interrupted sleep. In the SWAN study 37% of women between the ages of 40 and 55 reported difficulty sleeping, with highest rates noted in Caucasian and Hispanic women [22].
Sleep disturbances can be associated with VMS as well as psychosocial issues, such as stress- and other lifestyle factors. With more severe VMS, insomnia is much more likely, but not the sole factor. Poor sleep prior to the perimenopause transition is predictive of worsening sleep symptoms throughout menopause. Sleep symptoms tend to stabilize as a woman progresses through peri into the postmenopausal lifestage[23].
Depression, which can affect sleep, restless leg syndrome, and sleep apnea should also be ruled out prior to attributing sleep problems solely to hormone loss.
Mood and depressive symptoms are strongly associated with the perimenopause. The risk of adverse mood symptoms increased from 20% to 62% by the early perimenopause as compared to pre-menopause in the SWAN cohort. Three robust longitudinal studies–SWAN, the Penn Ovarian Aging Study, and the Harvard Study of Moods and cycles all demonstrated an increased risk for depressed mood during the menopausal transition, including increased risk of new-onset major depressive disorder and anxiety in women with no prior history of a psychologic diagnosis[24,25]. Peri and menopausal women were 2-4 times more likely to experience an episode, even when controlling for prior history of major depression, medication use, VMS, and upsetting life events[26]
In summary, like adolescence, the 10 years or so of perimenopause can be a difficult roller coaster of hormonal fluctuations and symptoms for women. It also presents challenges to providers in recognizing and diagnosing. Although we often think of VMS, GSM, Sleep disturbances and mood changes as symptoms of menopause, it is critical for us to incorporate the findings from the SWAN study to recognize that they typically occur in the perimenopausal phase as well, many years before the final menstrual period.
REFERENCES
- Dorr, B. “In the Misdiagnosis of Menopause, What Needs to Change? Am Journal Managed Care. September 14, 2022.
- Harlow SD, Gass M, Hall JE, Lobo R, Maki P, Rebar RW, Sherman S, Sluss PM, de Villiers TJ; STRAW 10 Collaborative Group. Executive summary of the Stages of Reproductive Aging Workshop + 10: addressing the unfinished agenda of staging reproductive aging. Menopause. 2012 Apr;19(4):387-95.
- El Khoudary SR, Greendale G, Crawford SL, Avis NE, Brooks MM, Thurston RC, Karvonen-Gutierrez C, Waetjen LE, Matthews K. The menopause transition and women’s health at midlife: a progress report from the Study of Women’s Health Across the Nation (SWAN). Menopause. 2019 Oct;26(10):1213-1227.
- Finkelstein JS, Brockwell SE, Mehta V, et al. Bone mineral density changes during the menopause transition in a multiethnic cohort of women. J Clin Endocrinol Metab 2008; 93: 861-8
- Paramsothy P, Harlow SD, Greendale GA, et al. Bleeding patterns during the menopausal transition in the multi-ethnic Study of Women’s Health Across the Nation (SWAN): a prospective cohort study. BJOG. 2014;121:1564–73
- Greendale GA, Sowers MF, Han WJ, et al. Bone mineral density loss in relation to the final menstrual period in a multi-ethnic cohort: Results from the Study of Women’s Health Across the Nation (SWAN).J Bone Miner Res 2012;27(1):111–8.
- Greendale GA, Huang MH, Cauley JA, Han W, Harlow S, Finkelstein JS, Hans D, and Karlamangla AS. Trabecular bone score declines during the menopause transition: Results from the Study of Women’s Health Across the Nation Trabecular Bone Score Study (SWAN-TBS). J Clinical Endocrinology and Metabolism 2020 April 4; 105(4): e1872-e1882
- Ishii S, Cauley JA, Greendale GA, Crandall CJ, Huang M-H, Danielson M, and Karlamangla AS. Trajectories of Femoral Neck Strength in Relation to the Final Menstrual Period in a Multi-Ethnic Cohort. Osteop Intl. 2013 Sep;24(9):2471-81.
- Shieh A, Karlamangla AS, Huang MH, Han W, Greendale GA. Faster Lumbar Spine Bone Loss in Midlife Predicts Subsequent Fracture Independent of Starting Bone Mineral Density. J Clin Endocrinol Metab. 2021 Jun 16;106(7):e2491-e2501.
- Randolph JF, Jr, Sowers M, Bondarenko IV, Harlow SD, Luborsky JL, Little RJ. Change in estradiol and follicle-stimulating hormone across the early menopausal transition: effects of ethnicity and age. J Clin Endocrinol Metab. 2004;89:1555–61
- Gallicchio L, Miller SR, Kiefer J, Greene T, Zacur HA, Flaws JA. Risk factors for hot flashes among women undergoing the menopausal transition: baseline results from the Midlife Women’s Health Study. Menopause. 2015;22:1098–107
- Avis NE, Crawford SL, Greendale G, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA internal medicine. 2015;175:531–9
- Freeman EW, Sammel MD, Lin H, Liu Z, Gracia CR. Duration of menopausal hot flushes and associated risk factors. Obstet Gynecol. 2011;117:1095–104.
- Smith RL, Gallicchio L, Miller SR, Zacur HA, Flaws JA. Risk Factors for Extended Duration and Timing of Peak Severity of Hot Flashes. PloS one. 2016;11:e0155079.
- Thurston RC, Sowers MR, Sternfeld B, et al. Gains in body fat and vasomotor symptom reporting over the menopausal transition: the study of women’s health across the nation. Am J Epidemiol. 2009;170:766–74.
- van den Berg MJ, Herber-Gast GC, van der Schouw YT. Is an unfavorable cardiovascular risk profile a risk factor for vasomotor menopausal symptoms? Results of a population-based cohort study. BJOG. 2015;122:1252–8.
- Szmuilowicz ED, Manson JE. Menopausal vasomotor symptoms and cardiovascular disease. Menopause. 2011;18:345–7
- Kim HK, Kang SY, Chung YJ, Kim JH, Kim MR. The Recent Review of the Genitourinary Syndrome of Menopause. Journal of menopausal medicine. 2015;21:65–71
- Avis NE, Brockwell S, Randolph JF, Jr, et al. Longitudinal changes in sexual functioning as women transition through menopause: results from the Study of Women’s Health Across the Nation. Menopause. 2009;16:442–52
- Avis NE, Green R. The perimenopause and sexual functioning. Obstet Gynecol Clin North Am. 2011;38:587–94
- Pettee Gabriel K, Sternfeld B, Colvin A, Stewart A, Strotmeyer ES, Cauley JA, Dugan S, Karvonen-Gutierrez C. Physical activity trajectories during midlife and subsequent risk of physical functioning decline in late mid-life: The Study of Women’s Health Across the Nation (SWAN). Prev Med. 2017 Dec;105:287-294..
- Kravitz HM, Joffe H. Sleep during the perimenopause: a SWAN story. Obstet Gynecol Clin North Am. 2011;38:567–86.
- Kravitz HM, Janssen I, Bromberger JT, et al. Sleep Trajectories Before and After the Final Menstrual Period in The Study of Women’s Health Across the Nation (SWAN) Curr Sleep Med Rep. 2017;3:235–50
- Bromberger JT, Kravitz HM. Mood and menopause: findings from the Study of Women’s Health Across the Nation (SWAN) over 10 years. Obstet Gynecol Clin North Am. 2011;38:609–25
- Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63:385–90.
- Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63:375–82
*This is Part I in a 3-part series focused on the Perimenopause
